The Sweaty Truth About Sleep Supplements, Night Sweats & Misdiagnosed Hormones
Dear midnight moppers, pajama peelers, and thermostat tango dancers,
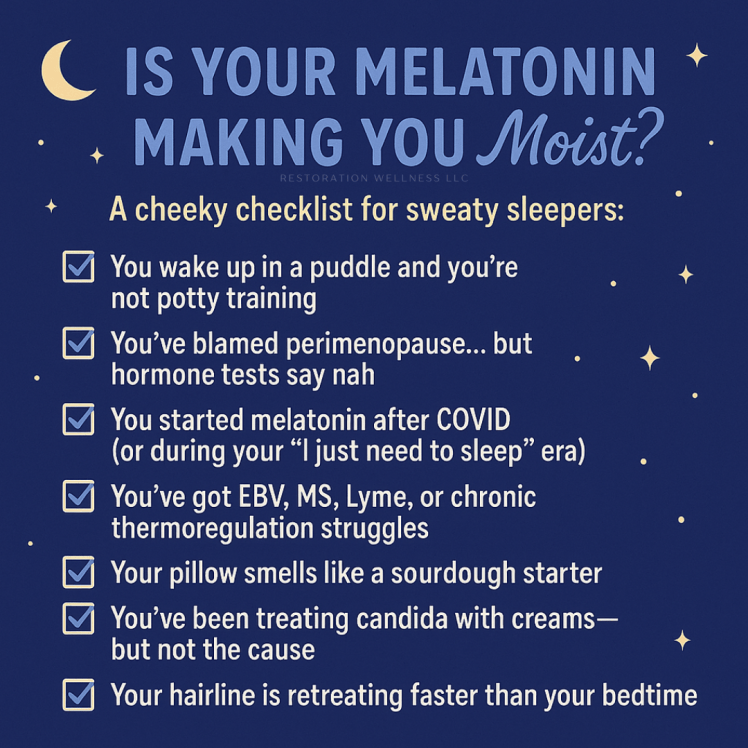
Let me talk about something that might just blow the covers off your nighttime mystery: melatonin. That sweet little hormone so many people pop like it’s a sleepy-time Tic Tac? It may just be behind your night sweats, misdiagnoses, and slow descent into skin yeast madness.
What I Thought Was Perimenopause Was Actually… Melatonin.
For four years after having COVID, I continued to suffer from relentless night sweats. We are talking sleeping-in-a-swamp-level moisture, people. Naturally, as a woman in her fabulous 30s/40s (don’t do the math, just go with it), the finger was pointed straight at perimenopause.
Doctors shrugged. Hormones tested “normal.” Still, I kept waking up soaked and suspicious.
Until one day, I had the audacity to stop taking melatonin. And just like that the night sweats ghosted me.
Mic drop.
How Melatonin Can Jack Up Your Temperature Regulation
Melatonin isn’t just a sleep regulator—it’s a neurohormone that can influence thermoregulation.
Here’s the geeky breakdown:
- It causes vasodilation, meaning it opens up your blood vessels to help your core temperature drop so you feel sleepy.
- In people who are temperature regulation-challenged (hello, MS/EBV/Lyme warriors), this drop can trigger an overcompensating body reaction—cue the night sweats.
- Add dysfunctional hypothalamus signaling (common in chronic infections and neurological disorders), and you’ve got a sweaty symphony playing nightly.
Your body’s doing its best, but melatonin’s like, “let’s lower the temp!” and your body’s like, “WE’RE FREEZING! SWEAT, SWEAT, SWEAT!” It’s a hormonal comedy of errors.
Why This Matters for Misdiagnosed Women
Because your sweat isn’t a menopause manifesto, it might just be a misunderstood molecule. Women are too often handed a “shrug and a script” when they walk into a doctor’s office with symptoms like:
- Night sweats
- Insomnia
- Fatigue
- Brain fog
- Mood swings
Cue the “It’s probably perimenopause” speech. And sure, that might be true sometimes — but not every time.
Here’s the problem:
We are more than hormones.
We are immune systems, neuroendocrine systems, and walking weather forecasts thanks to chronic infections like Lyme, EBV, mold illness, and post-viral syndromes (lookin’ at you, COVID).
And when a one-size-fits-all label like “perimenopause” is slapped on a complex picture, here’s what happens:
- Root causes are ignored.
- Supplement interactions (like melatonin) go unchecked.
- Helpful interventions (like detox support or neuroimmune care) get skipped.
- You get treated like a stereotype, not a whole person.
Even worse?
You might start HRT or antidepressants based on a guess. Meanwhile, that melatonin you are taking every night “just to sleep” is hijacking your thermoregulation system like a sweaty little saboteur.
Real Talk:
Misdiagnosis does not just waste time. It delays healing. It gaslights your intuition. And it creates cycles of symptoms that no one’s connecting, except you.
So, if you’re:
- Waking up drenched
- Getting passed around between specialists
- Feeling like “something isn’t adding up”
…it might be time to question the supplement, not the season of life.
Many people take melatonin long-term, especially post-COVID, where sleep disturbances ran wild. But no one stops to ask if it’s contributing to night sweats, thermoregulation issues, or yeast overgrowth.
Wait—Did You Say Candida and Hair Loss?
Yes, yes I did.
- Sweating increases moisture-loving skin yeast (candida).
- Candida on the scalp, chest, and neck? Itching, inflammation, and yes—hair loss.
- Add in compromised immunity from EBV/Lyme/MS and you have got a petri dish on your pillow.
It is not just a vanity issue. It is an inflammatory cascade.
Moral of the Midnight Story:
Melatonin isn’t always the hero. Sometimes it’s the saboteur.
Before you let someone slap a perimenopause label on your forehead or blame “hormones” for everything, check your supplement stack.
Especially if you’ve got:
✅ Post-viral fatigue (COVID, EBV)
✅ Chronic illness (Lyme, MS, autoimmunity)
✅ Neuroinflammation
✅ Thermoregulation issues
✅ A swamp for a bed
Mel’s Helpful Holistic Tips:
- Ditch the nightly melatonin and try magnesium glycinate, L-theanine, or passionflower instead.
- Support temperature regulation with adaptogens like ashwagandha (if tolerated) and cooling herbs like peppermint.
- Use antifungal skin sprays or powders on sweat-prone areas if you suspect candida.
- Rebuild the hypothalamus with phosphatidylserine, B vitamins, and lymphatic support.
Final Word: You’re Not “Crazy,” You’re Just Well-Researched.
And maybe now a little bit drier. Drop the melatonin, not your sanity. And for the love of sleep (and dry sheets), let’s start normalizing the conversation around misdiagnosis, misunderstood supplements, and the very real bio-individual chaos happening under the hood. You’re not broken—you’re just finally asking the right questions.
So go forth, spread the sweaty gospel, and maybe—just maybe—help another poor soul out there realize their night sweats aren’t hormonal doom… they’re just a hormone hijack in a tiny capsule.
Share this. Save someone’s sanity. And maybe their pillow, too.
Need help untangling your supplement chaos or hormone hysteria? Book a session through my client portal and let’s get you sorted—no sweat!!
👉 Client Portal
Discover more from Restoration Wellness, LLC
Subscribe to get the latest posts sent to your email.